By Prabhat Prakash & Prarthana Sharma
Mumbai: Clinical research is a complex process that necessitates cooperation between many parties to guarantee patient safety, moral behaviour, and effective medication development.
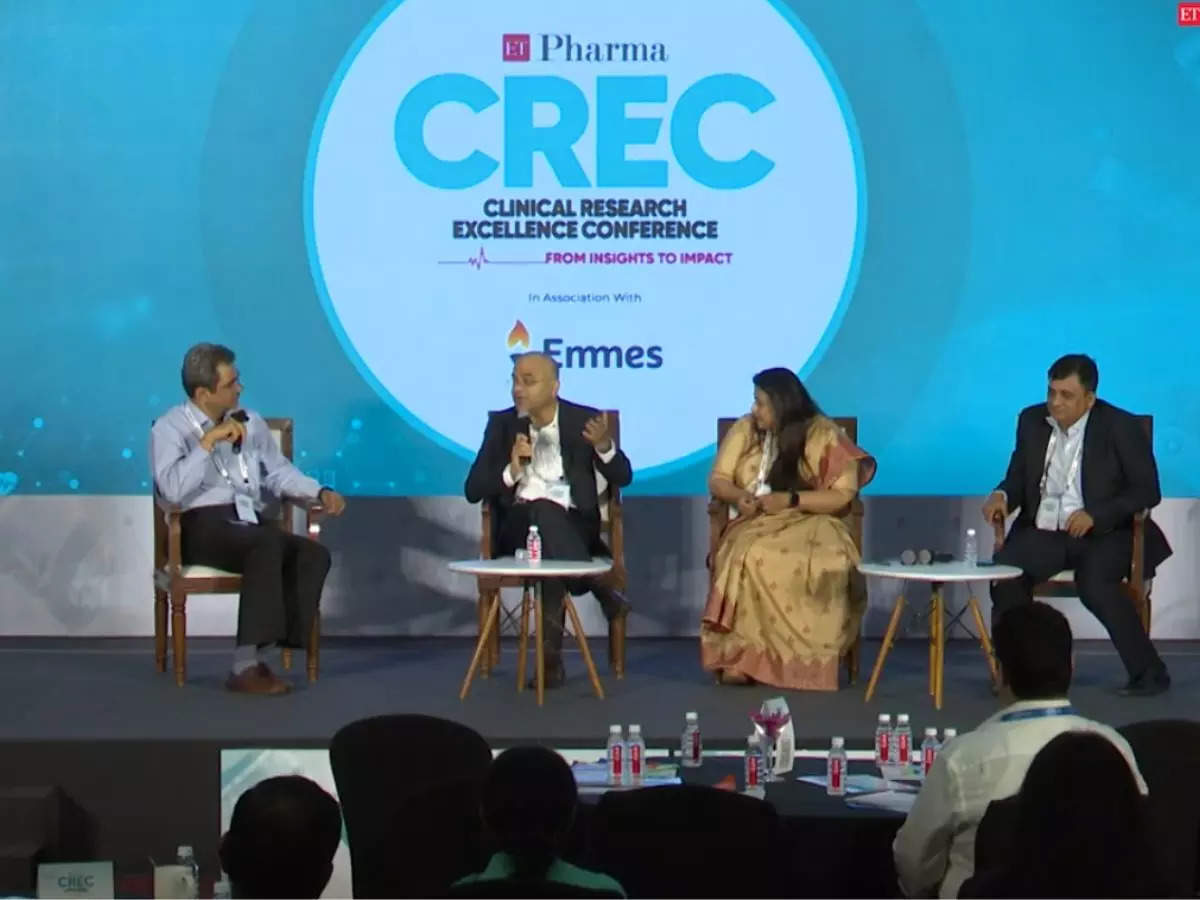
Professionals in the sector covereged at ETPharma’s Clinical Research Excellence Conference (CREC) 2024, where they discussed how important it is to involve a variety of stakeholders, such as advocacy groups, regulators, and patients, during a panel discussion titled ‘A Multi-Stakeholder Perspective on Integrating Clinical Research into the Continuum of Care’. The discussion focused on issues and prospects concerning pharmacovigilance, access to novel medications, and clinical trial management, finally pointing to practical ways to make improvements.
The participants for the discussion were Dr Shubhadeep Debabrata Sinha, Senior Vice President & Head (Global) – Clinical Development & Medical Affairs, Hetero Labs Limited; Suneela Thatte, VP and Head-Healthcare R&D India, Merck Group; and Dr Avinash R Kakade, Sr Vice President Global Head of Pharmacovigilance, Dr Reddy’s Laboratories. Dr Jaideep Gogtay, Global Chief Medical Officer, Cipla Ltd moderated the discussion.
Highlighting the clinical development, Dr Gogtay said, “In clinical trial protocols, the patient’s viewpoint is important but frequently disregarded. Throughout my vast experience spanning more than a hundred trials, I have faced a variety of obstacles in bringing stakeholders together in pursuit of the shared objective of creating novel medications for illnesses. Aligning the varied interests and priorities of stakeholders, from scientists and researchers to patients and representatives of society, remains a formidable challenge. Whether it’s patient safety, societal effect, or scientific rigour, every stakeholder group has unique concerns. It takes good communication, open decision-making procedures, and a common dedication to furthering medical research for the benefit of patients and society at large to reach an agreement amongst these disparate points of view. It is imperative to incorporate the patient’s voice at every stage of the drug development process, not just for moral considerations.”
Thatte emphasised, “The complex network of interested parties in clinical research highlights the importance of the field to society. All the aspects that go into taking medicine from concept to clinic are involved, from the early phases in the lab to the ethical concerns of regulators and researchers. But in all the excitement about deadlines and new technology, the patient’s viewpoint is frequently neglected, which creates problems with recruitment and unworkable procedures. Since patients are important stakeholders, industry professionals should give their feedback top priority when doing research. To improve illness management and general well-being, strengthening the patient pillar entails incorporating their input into study design and adopting a comprehensive approach to patient care that goes beyond clinical outcomes.”Explaining in the perspective of the pharmaceutical industry, Dr Sinha said, “Navigating the complex route of clinical trials and product development in the pharmaceutical sector is similar to threading a needle through a maze. At its centre is the critical decision-making process of selecting the correct drug for the right patient, which is a hard undertaking. The initial challenge is to identify society and patient requirements, which are sometimes concealed by a lack of public knowledge. Bridging this gap requires proactive engagement with patient advocacy groups as well as direct patient connections. Even with promising medication in hand, the trip is plagued with challenges.”
Dr Kakade said, “Working internally within a corporation, particularly in a function that requires cooperation across various departments, presents several obstacles. Meeting deadlines established by the Chief Regulatory Officer (CRO) or partners necessitates ongoing communication and engagement. One important part is to communicate with investigators to hear their perspectives while also ensuring the trial’s integrity and ethics are maintained. This could include comprehensive discussions to clarify causal analyses or navigate decision-making processes. Furthermore, securing internal clearances can be difficult, with important stakeholders such as the IT department critical to database functionality, especially when dealing with remote offices like those in Delhi. Former issues, such as the lack of simplified reporting systems, complicate matters.”
Dr Sinha continued, “Post-trial access to investigational medications is an important but frequently disregarded feature of clinical studies. While standards exist, there is debate about whether patients should have access to the therapy if it provides more benefit than past therapies. Medical affairs departments play an important role in this phase by organising structured activities such as patient access and outreach initiatives, particularly for life-saving medications like those used in oncology. Patients who participated in trials frequently become advocates for these drugs, and pharmaceutical corporations often support them after the trials. Pharmacovigilance activities, such as post-marketing studies, help to ensure the drug’s safety and efficacy in real-world settings.”
Thatte said, “Patient advocacy organisations play an important role in the healthcare scene, particularly in countries such as India, where their influence extends beyond uncommon diseases. These organisations act as important liaisons between patients and pharmaceutical corporations, providing critical insights into patient experiences and needs. Pharmaceutical businesses can acquire valuable data on the effectiveness and accessibility of their medications by actively engaging with these communities. Finally, this collaboration assures that scientific advances in medication development result in practical advantages for patients, emphasising the importance of such interactions in enhancing healthcare outcomes.”
Dr Gogtay emphasised that an important feature of medicine is access and availability, particularly in countries like India where such programmes have had a considerable impact. Allowing patients access to treatments that are still in the clinical trial phase can save lives, as seen by the success examples cited. The ability to provide these treatments before formal clearance highlights the need to balance regulatory processes with patients’ urgent medical needs. This strategy necessitates a shift in mentality among pharmaceutical corporations, regulatory authorities, and healthcare practitioners. As awareness increases, there is a clear need for education and advocacy to ensure that life-saving therapies are available when and where they are most needed, highlighting the necessity of patient-centred healthcare policies.