Your support helps us to tell the story
This election is still a dead heat, according to most polls. In a fight with such wafer-thin margins, we need reporters on the ground talking to the people Trump and Harris are courting. Your support allows us to keep sending journalists to the story.
The Independent is trusted by 27 million Americans from across the entire political spectrum every month. Unlike many other quality news outlets, we choose not to lock you out of our reporting and analysis with paywalls. But quality journalism must still be paid for.
Help us keep bring these critical stories to light. Your support makes all the difference.
This story is part of an investigative series and new documentary, The A-Word, by The Independent examining the state of abortion access and reproductive care in the US after the fall of Roe v Wade.
Erica Allen was terrified and in agony last April at a Delaware hospital just before the emergency birth of her fourth child, fully aware of the dangers of being a Black mother in America. She kept thinking about her cousin: a Black doctor who’d collapsed at the mall and died while pregnant two years earlier, losing the son she’d already named Cruz.
“It doesn’t matter how educated you are,” Erica, a nurse and doula, tells The Independent. “It doesn’t matter whether you graduated college, medical school, dropped out … just the color of your skin could impact the outcome.”
Erica’s first birth nearly 20 years ago had been traumatic, too; her body was so swollen with pre-eclampsia as she arrived at the ER at 35 weeks that her own mother didn’t recognize her.
Erica was monitored particularly carefully by her medical team before the 2023 birth of her fourth child, but she was also tracking her own blood pressure. She’d become intimately familiar with her usual levels and noted a concerning rise towards the end of her pregnancy.

When she raised it with her medical providers, they dismissed it because she was within the normal limit — even if the numbers were unusual for her. Until one day her blood pressure spiked suddenly, forcing an emergency induction after which Erica suffered the first postpartum hemorrhage of her four deliveries, suffering significant bleeding and blood clots.
“I wasn’t heard,” says Ms Allen, 42, as her 18-month-old plays in the background. “I really was not heard.”
She’s echoed almost verbatim by another Black mother 160 miles north in Brooklyn — who made nearly a dozen medical visits to report bleeding and intense pain during her 2022 pregnancy, before a third ER trip finally identified a life-threatening ectopic situation.

“I didn’t feel like I was being listened to,” Ashley Simpo tells The Independent. She’d given birth to her son a decade earlier and things felt vastly different this time around.
“I knew in my body something wasn’t right,” Ashley says. “The bleeding continued, and I had to make a fuss to get anybody to follow up with me.”
The mothers’ stories mirror a narrative heard time and time again from Black women across America whose lived traumas evidence a stark statistical reality: Black maternal healthcare and morbidity in the US remain wholly unequal in comparison to the experiences of everybody else.
On all key data points, Black women have worse pregnancy outcomes than any other racial group, with Native American women close behind. Black women are more likely to die in childbirth, more likely to have preterm babies, more likely to have complications and more likely to have their babies die.
Black women know these risks — and advocate fiercely for themselves and their babies. But time and time again, their concerns are ignored, with often deadly consequences.
By the numbers
The stats are horrifying. Black women in the US are 2.5 times more likely to die from pregnancy-related issues than white women.
That means 49 Black women die per every 100,000 live births, according to the National Center for Health Statistics (NCHS). The maternal mortality rate for white women is 19 deaths per 100,000 live births, a figure which is even lower for Hispanic and Asian births.
Infant mortality is also twice as high for Black babies as for white babies, with 11 Black babies dying per 1,000 births, compared to four white babies.
Why do Black women and babies have such dire maternal health outcomes in this country? As summed up by the CDC, “multiple factors contribute to these disparities, such as variation in quality healthcare, underlying chronic conditions, structural racism, and implicit bias.”
“When there is poor access to care, that is a driver of poor maternal health outcomes. However, that’s only part of the story,” says Dr Amanda Williams, a leading OB-GYN with decades of experience and the chief medical officer at maternity healthcare charity March of Dimes.

Going a step further, Dr Williams blames “straight racism” as one factor — warning against dismissing racial healthcare disparities as purely socioeconomic consequences.
“Even when you adjust for access and adjust for income, you still have that discrimination and still have that increased risk,” Williams, a professor of obstetrics and gynecology at Stanford University, says. Both data and anecdotal evidence back that up.
Money alone does not protect Black women. In fact, in California, death rates among the richest Black mothers were even higher than white mothers in the poorest socioeconomic group, according to a 2023 study by the National Bureau of Economic Research (NBER).
A similar trend was found when comparing infant mortality rates of Black and white babies across socioeconomic groups.
The authors of the NBER study say that no one factor can explain the disproportionality, but suggest that policy-induced racial segregation and cumulative stress due to racial discrimination are likely causes.
Erica points to her doctor cousin who tragically died during a high-risk pregnancy; already mother to a young daughter, the 34-year-old suffered hypertension and collapsed while shopping. Doctors delivered the son she’d already named Cruz, but he survived only five days.
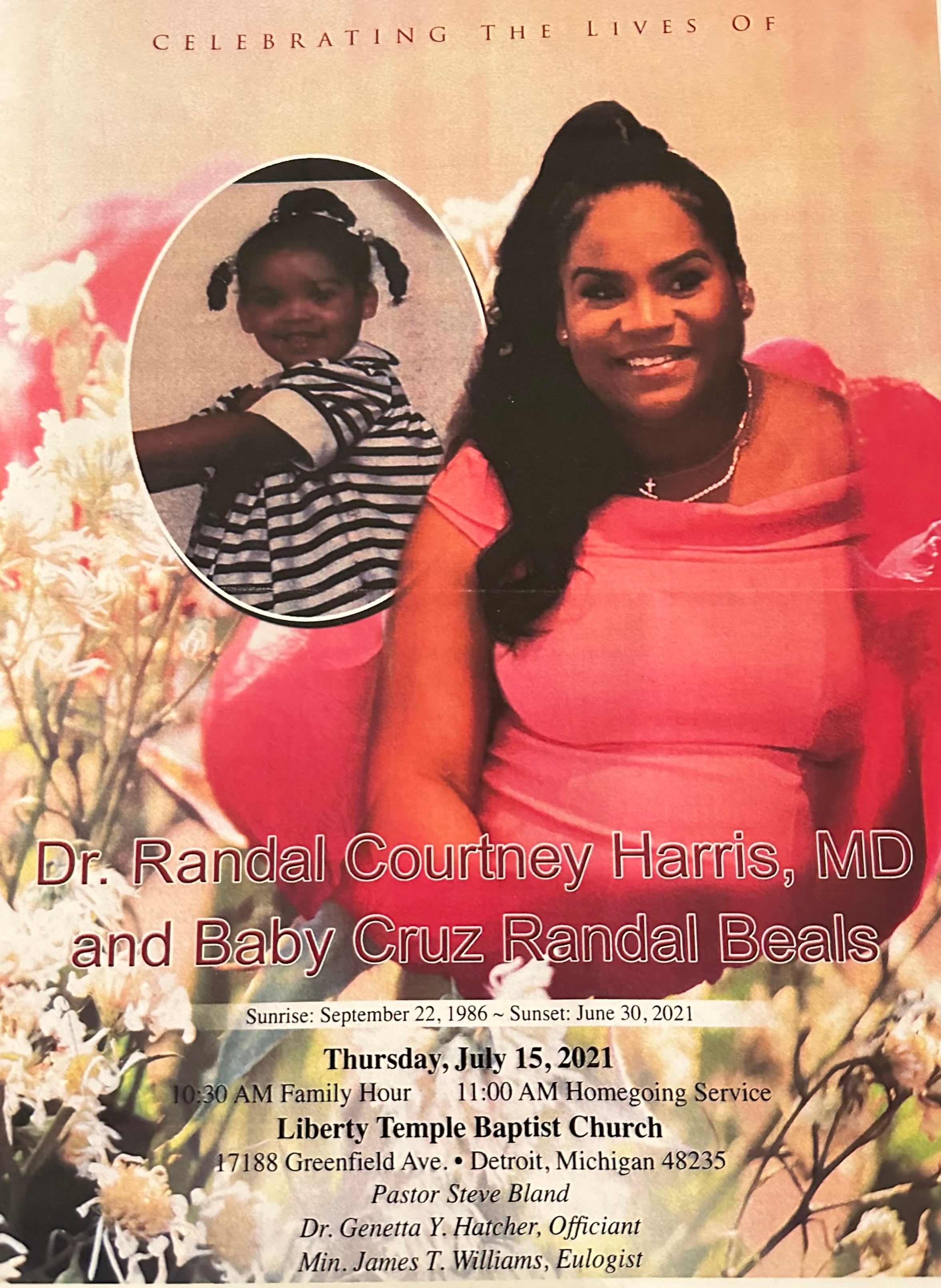
The pair were remembered in a joint service later that month in July 2021.
“The fact that she’s a doctor and it happened to her … a lot of times you’ll hear people try to put it on socioeconomic disadvantage,” she tells The Independent. “Now, it doesn’t matter how educated you are.”
One of the highest-profile birth trauma stories from a Black mother also comes from one of the most famous female athletes on the planet: Serena Williams, who first detailed in a 2018 Vogue interview how she’d nearly died after giving birth to her daughter Olympia the year prior.
Williams, on high alert because of her history of blood clots — a history known to her medical team — suffered excruciating pain postpartum and felt like she was “dying.”
Like the women The Independent spoke to, medical professionals ignored Serena when she realized something abnormal was happening with her body and raised it to them.
Serena went so far as naming the exact scans she needed to save herself, even then being initially shot down.
“In the other room, I spoke to the nurse. I told her: ‘I need to have a CAT scan of my lungs bilaterally, and then I need to be on my heparin drip,’” Serena recounted in a 2022 Elle essay. “She said, ‘I think all this medicine is making you talk crazy.’”
When the nurse eventually told the doctor and the scan was ordered, she wrote: “I had a blood clot in my lungs, and they needed to insert a filter into my veins to break up the clot before it reached my heart.”
Serena spent six weeks in bed recovering. For the birth of her second daughter, a scheduled c-section, she had four doctors on call.

“These are affluent people with money. So what do you think it looks like for those that don’t [have money], right? For those in the working class or in poverty, who are every day just working to live,” says Cortes Maria Lewis James, a trained nurse and doula for the Southern Birth Justice Network, a Florida-based pregnancy group that provides midwife and doula care, advocating for maternal care accessibility for people of color and LGBTQ+ individuals in particular.
Black women are also more likely to have their births financed by Medicaid – 64 percent in 2021, compared to 28 percent for white mothers, according to the CDC.
As a freelance writer who was on Medicaid at the time of her 2022 ectopic pregnancy, Brooklyn mom Ashley felt her lack of insurance meant she got lower-quality care.
“I absolutely feel that I was not treated in the same way [as those with insurance],” she tells The Independent. “When I went to see the doctors, they were telling me what was wrong, not asking me. I wasn’t really heard.”
“Sometimes I’ve had access to the best insurance and the best doctors, and there’s times I don’t … and I notice the difference.”
Abortion as healthcare
Since Roe v. Wade was overturned, Black women in states with abortion bans may be facing some of the worst impacts, exacerbating existing divisions in maternal care.
A new report on maternal care post-Roe tracks detailed cases where care standards have dropped in states impacted by abortion restrictions, since September 2022. Nearly a quarter (24 percent) of cases analyzed involved a Black mother, though they make up just roughly 14 percent of births.
In 2021, Black women accounted for 42 percent of all abortions in the US. If impeded access to safe abortions means that more Black women are likely to go ahead with their pregnancies, the state of maternal healthcare shows that these same women are at far higher risk of poor care.
“The effects follow marginalized communities in the worst way, and Black and brown folks in the worst way,” James says. “Now you’re forcing people into birth.”
Grieving mother Nicole Blackmon experienced that firsthand in the most tragic of circumstances two years ago. Her teenage son, an innocent bystander, had just been killed in a drive-by in Alabama, and she found herself pregnant with a “miracle” child months later.
Blackmon and her husband decided to move to Tennessee for a new start — but were informed by doctors soon after arrival that her baby suffered from a lethal condition in which the organs develop outside of the body. She was told her child would not survive, and the pregnancy — already complicated by a number of underlying conditions — was threatening her life, too.
A genetic counselor advised her to get an abortion. But Tennessee’s draconian abortion laws made that impossible, and Blackmon was neither healthy enough nor financially able to travel out of state.
“It was like, ‘Are you serious?’” Nicole tells The Independent. “‘There’s no loophole or anything to try to save me or women that are in my situation? I’m about to die, and you’re telling me that, because of a law, I’m unable to get treatment or help?
“I felt like nothing,” she says.

She and her husband did the research, crunching the figures to travel to a different state where abortion would be legal, how much it would cost to take time off work and pay for hotel, transportation and food. “No one talks about all of that,” she says.
Instead, while grieving the loss of another son, she gave birth to stillborn Ethan, whose tiny body she was too traumatized to see or hold after delivery.
The new laws, says Florida nurse and doula Cortes, necessitate people “leaving the state … but marginalized folks don’t have access to that right.
“Black and Brown folk don’t have the money, don’t have the access, to do that.”
Channeling trauma into care
Ashley feels that medical professionals gave less credence to her concerns because she’s Black — and sees this as a risk to pregnancy care more widely.
“Race absolutely plays a part, in terms of being met with someone assuming your ignorance, because of bias,” she says.
“I don’t think that a lot of doctors are asking Black women how they’re feeling. If they’re feeling stressed, if they feel safe, if they’ve been eating, all of those things that tie into whether or not their pregnancy is going to be healthy.”
Discrimination has been shown to cause inaccurate pain assessment for Black patients; which, separately, means Black patients are also 22 percent less likely to receive pain medication, according to an analysis of two decades of pain studies.
Having more Black people working in medicine is one step towards improving Black maternal health outcomes — and the data shows its works.
A 2020 study showed that Black babies were less likely to die when cared for by Black physicians.
For this reason, says Dr Williams, “it actually is a matter of life and death importance.”

Suffering birth trauma inspired Erica and Ashley to advocate for others. Following the birth of her third child, Erica studied to become a nurse, connecting her own experiences to the statistical and anecdotal evidence she’d seen on racial disparities in maternal care.
She became particularly interested in how doulas — non-medical professionals trained to assist before, during and after birth — can address that inequality, starting the nonprofit Do Care Doula Foundation in 2021.
“There were doulas that wanted to train, and the trainings are expensive,” she says. “Also, the people that we want to support, the Black and brown birthing community, can’t always afford … doula support services.”
Her foundation also provides community outreach and awareness about everything from safe sleep to lactation.
In Brooklyn, Ashley says guidance from a doula helped her get through the ectopic pregnancy without surgery and connected her to various forms of support — motivating her to train to be a doula now, too, citing the need for and benefits of holistic care.
“I felt compelled, especially when Roe v Wade was overturned, to be part of the movement in a way that is supportive for my community, and wanting to be that resource for whoever can’t find it anywhere else.”
In Florida, Cortes is taking her role as a community support and resource even further — helping patients as a “full-spectrum doula … preconception all the way to postpartum, including abortion doula, if necessary” and also fostering a baby whose mother is homeless and lost custody.
“Here is a Black boy with all of these medical issues and a mother, a Black mother that is struggling to just live life and systems of oppression that cannot even give her what she needs,” says Cortes.
The child’s birth mother is again pregnant — so Cortes has also now been called upon by authorities to foster the boy’s new baby sibling.
“It’s just a cycle,” she tells The A-Word. “And my husband said to me two days ago, ‘So what’s going to happen if she just keeps having kids?’”
The strict new laws are life-threatening, but there’s also a monumental ripple effect across public services and the wider community.
“The foster care system is not prepared,” she says, pointing out that “when you’re stuck, with an extra mouth to feed, guess where the baby goes? In the foster care system.”
As she sees the results on the front lines, Cortes can’t help but think about the people who enabled it all in the first place.
“How could you sit and write that legislation? But secondly, how could you support it?” she laments to The Independent. “Are you that blind to the challenges of marginalized communities?
“Or do you not care?”





